Safety is the cornerstone of any clinical trial, ensuring that participants are protected while contributing to medical advancements. Clinical trials are carefully structured to assess not only the effectiveness of new treatments but also their safety profile. As new therapies, drugs, or devices are being tested, rigorous safety protocols are in place to minimize risks to participants. This blog post explores the essential role of safety in clinical trials, what measures are taken to protect participants, and why these safeguards are crucial for the success of medical research.
1. Thorough Pre-Trial Testing and Screening
Before a clinical trial even begins, extensive pre-trial testing is conducted to ensure that the treatment or intervention is as safe as possible. Researchers perform laboratory and animal studies to identify potential risks and to determine how the treatment behaves in different conditions. Participants are also carefully screened for any pre-existing health conditions or risk factors that could impact their safety during the trial. This screening process helps identify who may be suitable for the trial, ensuring that only individuals who meet specific health criteria are enrolled, minimizing any potential harm.
2. Informed Consent: Understanding Risks and Benefits
One of the most important safety measures in clinical trials is informed consent. Before participating, individuals are provided with detailed information about the trial, including the potential risks, benefits, and any possible side effects of the treatment. This ensures that participants are fully aware of what they are agreeing to and can make an informed decision about whether to proceed. By understanding the trial’s scope and potential impacts on their health, participants are empowered to ask questions and voice concerns, which is a critical part of the safety process.
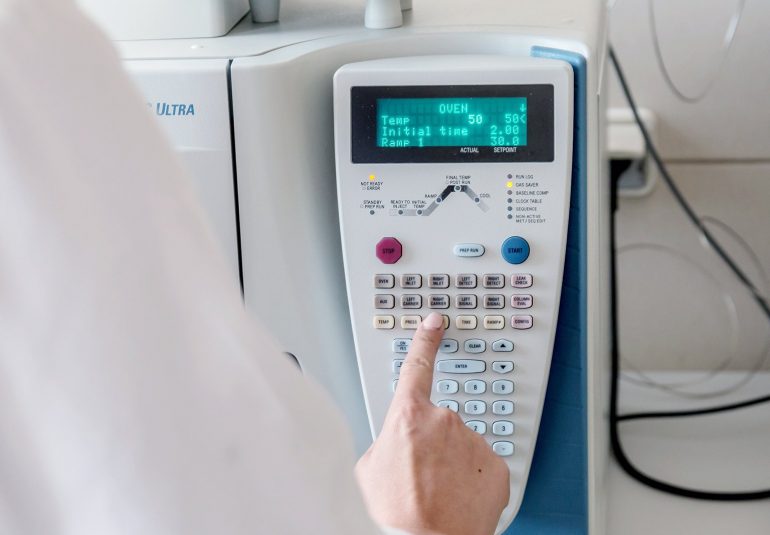
3. Ongoing Monitoring of Participants
Once a clinical trial is underway, the safety of participants is continuously monitored. Researchers and healthcare professionals track participants’ health and closely observe any adverse effects that may arise. Routine check-ups, laboratory tests, and diagnostic screenings are conducted throughout the trial to monitor participants’ well-being. If any safety concerns arise, such as unexpected side effects or complications, researchers are equipped to adjust the treatment plan or discontinue the trial to ensure participant safety. This proactive monitoring is vital for preventing any potential harm.
4. Independent Oversight and Ethical Review
Clinical trials are subject to strict ethical standards and oversight by independent review boards, also known as Institutional Review Boards (IRBs). These boards consist of medical professionals, ethicists, and community members who evaluate the trial’s design, risks, and safety protocols before it begins. The IRB ensures that the trial is conducted ethically and that the safety of participants remains the highest priority. They also continue to review the trial’s progress periodically, ensuring that all necessary safeguards are in place and that participants’ rights are respected throughout the process.
5. Risk-Benefit Balance
In clinical trials, there is always a careful balance between risk and benefit. While every medical treatment carries some level of risk, researchers aim to minimize potential harms while maximizing the benefits. The safety of participants is considered in every aspect of the trial design, and no trial moves forward unless the potential benefits outweigh the risks. It is important to note that clinical trials also provide new treatments to individuals who may not have access to other therapies, giving participants the opportunity to benefit from cutting-edge medicine that could significantly improve their health.
6. Transparency and Reporting of Adverse Events
Transparency is key to ensuring safety in clinical trials. All adverse events, no matter how minor, are carefully documented and reported. This transparency helps researchers understand the risks associated with a treatment and identify any potential issues before they escalate. If an adverse event occurs, the data is shared with regulatory bodies like the FDA (Food and Drug Administration), ensuring that all findings are made available to the broader medical community. This information is crucial for ensuring that treatments are safe for the general public once they are approved for widespread use.
7. Post-Trial Safety and Long-Term Monitoring
Even after a clinical trial concludes, safety continues to be a priority. Post-trial monitoring is crucial for understanding the long-term effects of a treatment. Participants may be asked to continue follow-up visits to ensure that any delayed side effects are detected and addressed. In some cases, treatments approved in clinical trials may still undergo ongoing safety studies to track their long-term effects as they become available to a larger population. This continuous monitoring ensures that the safety of participants and future patients remains a central concern.
Conclusion
Safety in clinical trials is not only about protecting participants—it’s about ensuring that the data collected is reliable and that medical advancements are grounded in research that prioritizes well-being. From rigorous pre-trial testing to ongoing monitoring and independent oversight, clinical trials are designed with participants’ safety in mind at every step. If you are considering participation in a clinical trial, you can be assured that the process is built with your safety as the top priority. Through these critical safety protocols, clinical trials continue to advance medical knowledge while safeguarding the health of those involved.